Growing up, I always had ‘tummy problems’. Since as far back as I can remember, I would spend endless hours stuck in the bathroom, having stomach cramps and struggling to eat. My weight would fluctuate up and down, and throughout my childhood I had multiple hospital stays for my supposedly ‘lazy’ bowels.
Despite years of tests, being seen by paediatric gastroenterology consultants and a near-constant stream of laxatives – nobody could come to a satisfactory answer as to what was causing my issues and I was told repeatedly that I’d likely outgrow my symptoms in time (spoiler alert, I never did!). Through paced eating, avoiding flare foods and frankly, having a lot else going on to distract me, I managed to cope relatively well with my symptoms throughout my teens – accepting the fact that there were days where I’d feel terrible for no reason, and never quite being sure when a flare would strike.
In 2020, during the pandemic, I got married and moved in with my wonderful Husband. Being vulnerable due to my other conditions, I ended up leaving my corporate job and working from home, setting up my own company – Inkfire. This was good for me, as for the first time I got to sit back and look at how some of my symptoms were affecting me in a much clearer way, but it became evident that my digestive issues were worse than I had been making out. Still, I didn’t think much of it. After all, I’d been told this was just ‘how I am’.
Then, roll on January 2021 and a sudden change in my symptoms. Overnight, my digestive issues got a lot worse, rushing to the bathroom multiple times per day, losing blood and discomfort both when I ate, and when I didn’t. I’d never had such severe physical symptoms before from my stomach, and I was really shocked at how quickly things got worse. However, being chronically ill, you get used to your body having these kinds of flares and so I didn’t rush to get it checked.
2 weeks in, I decide to notify my GP of my symptoms, as they were not improving. I have a telephone consultation due to COVID. I had no idea what to expect, or what tests to push for, so I went into this completely blank. The Doctor asked me some basic questions but did not suggest doing any tests. He thought that my symptoms were likely due to diet and advised that I up my fibre and see if I improve. I was told to ‘help myself’. Something I have been told oh to many times in my time with chronic illness.
Undoubtedly, I wasn’t feeling very validated. I started to think that I was making these symptoms up in my head, even as they continued and worsened over the coming months. Slowly, nausea started to creep in on a daily basis and I was finding that I wasn’t enjoying food. I also started to develop food allergies to things I’d never had an issue with. Eating was becoming a minefield, no matter how much fibre I ate. I tried different diets, nothing helped.
It wasn’t until around 3 months later (and some very scary Google searches!) that I finally decided enough was enough. One day, I was stuck in the bathroom for more than 3 hours, bleeding excessively and feeling sick. I contacted 111, who directed me to attend my local A&E. I hoped that this was going to be the beginning of proper investigation, but sadly that was not what happened. Perhaps a story for another day, but to summarise the A&E department I attended took over 8 hours to see me, had no beds and were very short-staffed. They did run my bloods to check if I was anaemic, but at that time I wasn’t. The triage nurses seemed very concerned by my symptoms, but unfortunately, the on-duty Doctor was much less invested.
The Doctor refused to refer me to the gastroenterology team after seeing my blood results. He did a physical examination but then decided that my symptoms were due to Hemorrhoids (a common misdiagnosis). He told me that he felt that I was being ‘dramatic’ and that it was highly unlikely someone of my age would present with severe issues, so he sent me home and once again told me to learn to live with this. By this point, I was feeling rather stupid.
Once again, I tried to manage my symptoms at home for many more months. During this time, I had some quite major issues with my other conditions, including severe UTI’s, a broken rib and arthritis flare-ups. Each time I was seen at the hospital or GP, the Doctors would acknowledge that something was wrong digestively, but it would never turn into any more than that.
Finally, flash forward to May 2023 and my symptoms were the worst they’ve ever been. I’d lost weight, my hair began falling out, I was constantly nauseas and even things that I once considered ‘safe foods’ were causing excessive bloating, pain and sickness. I was at my wits end physically and emotionally. I couldn’t leave the house without having an accident. I once again decided enough was enough and made an appointment with my GP.
My appointment comes about 3 weeks later, after having had some bloods done. This GP took the situation much more seriously because I was much more determined that I needed support and agreed that something wasn’t right as she could see that I was suddenly very anaemic. However, throughout the appointment, the GP reiterated many, many times that she felt it was ‘very unlikely someone of my age had any ongoing issues’ and that the anaemia was ‘likely due to my age and having a menstrual cycle’ leaving me once again questioning if I was doing the right thing. This GP referred me to the hospital, to the Colorectal department for urgent investigation. This was the kickstart of me getting much better care.
Just 2 weeks later, I received a letter requesting that I have a colonoscopy from this department. Now, for various reasons which I’ll go into another day, I didn’t feel physically able nor safe to have a colonoscopy (my other condition hEDS causes tearing) so instead, a CT Colonoscopy was arranged. This was an unpleasant test, however, so useful. 3 weeks after having the test, I received a phone call from the Inflammatory Bowel Disease nurses, confirming that I have very severe Pancolitis. I was not expecting such a quick outcome, let alone via a phone call and the relief to know that they’d found something was HUGE. I cried with relief. After years of questions, finally proof that this wasn’t all in my head.
Over the coming weeks, I had a bit of a crash course in Pancolitis. In brief, it’s a form of Ulcerative Colitis that affects you’re entire colon, causing a huge amount of inflammation and ulcers. Pancolitis develops over time, so the delay in getting treatment, I have discovered likely contributed to how bad my Pancolitis has become. A lesson if you ever needed one to push for help when you feel that something’s not right. I was given some medication to trial, that being Mesalazine which has been helpful. I also did a number of other less invasive tests to help the hospital determine the severity of my UC, including bloods, stool samples and similar.
Around a month later, I met with my Consultant for the first time. It was at this appointment that he answered many, many of my questions and gave me a bit more of an insight into what to expect from my UC. He made it clear, that for some surgery is the only option long-term, but that there are medications to try in the meantime. He shared that my stomach inflammation levels were exceedingly high, at that time around 2300, when the ‘safe’ figure is 100. So clearly, I had some a massive fight going on inside of me. One of the things that I’ve been very concerned about is my malabsorption and hairloss, so this was raised with him with the hope that it will improve. So far it hasn’t.
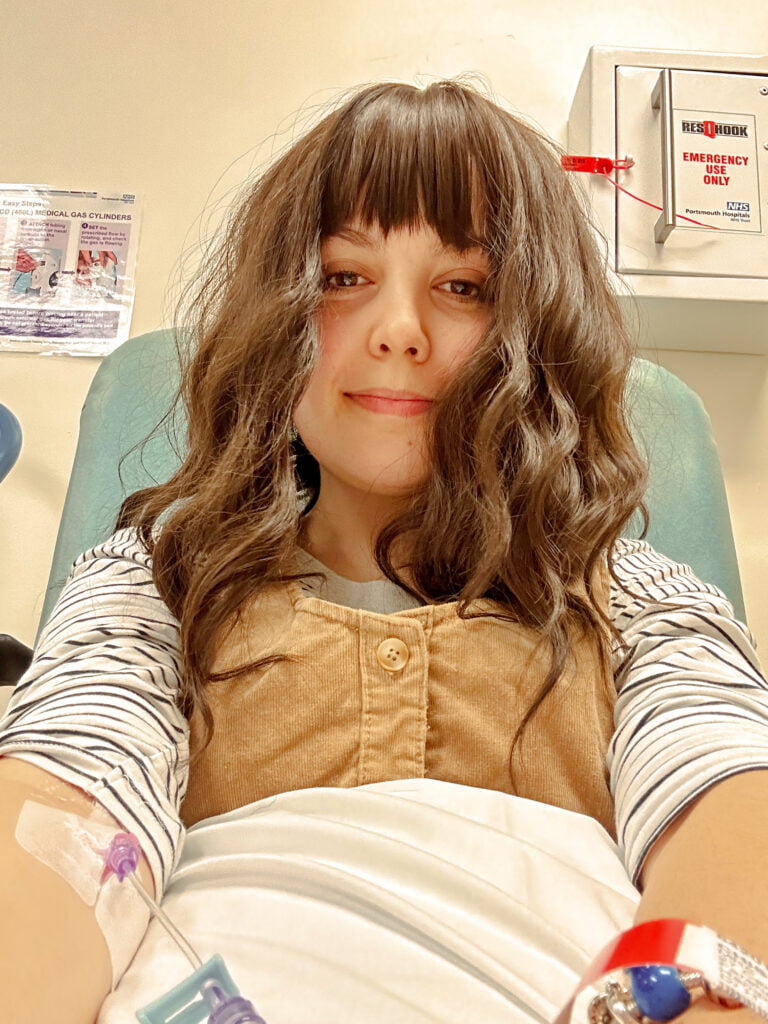
An action plan was agreed, to trial me on Prednisone steroids during September and October 2023, as well as allow me to have 2 iron infusions to help my anemia. I was also asked again if I’d be willing to have a colonoscopy, but managed to agree upon a Pillcam endoscopy instead. I’m happy to talk more about this, if anyone is interested in a separate post.
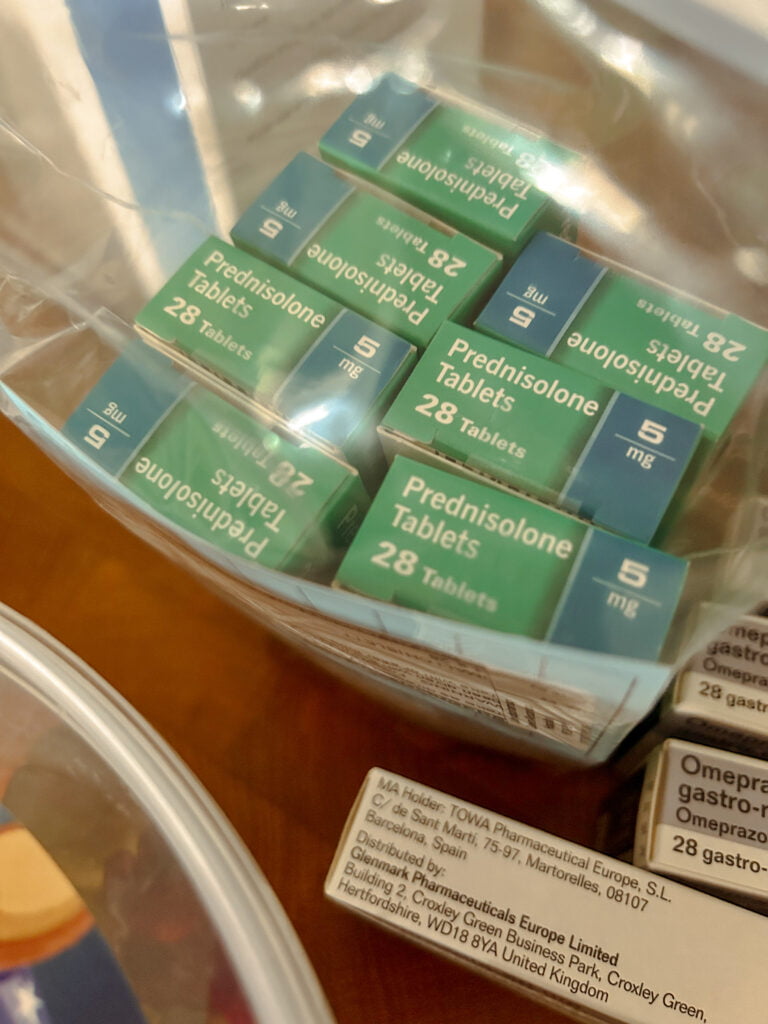
During September, I began the steroids, and at first they really worked. For the first time in years, I had a break from my symptoms, I could eat again and I felt genuinely better. This combined with the Iron infusions meant that I was actually feeling almost human! Sadly though, you can’t stay on steroids long term as it’s extremely bad for your bones and so you have to taper your dosage. As I have been tapering, my symptoms started to come back and this was compounded by the preparation for the Pillcam stripping my stomach and making me really quite unwell. So, at the end of September, I had to put my steroid dosage back up while in an emergency appointment with 111 and at the moment, I’m waiting to hear more about long-term care. Since returning my steroids to a slightly higher dose, I have returned to feeling much better, so currently this is the best management I have.
There are a variety of options I’m told that you can pursue before surgery becomes the only option, including oral steroids, IV steroids and infusions. At the moment, I believe that infusions are the route we’re looking at next, so I have a lot to learn about those. I’m still very new to the world of Ulcerative Colitis, but this has been my experience so far. There have been some big ups and downs, and the NHS does an amazing job of supporting but the funding and resources allocated to IBD are very limited.
Alongside the medication, I have also been trying to do what I can myself to support my body, including starting an anti-inflammatory diet and trialling turmeric capsules for inflammation. I’m waiting for my next inflammation test results to hear if these are helping.
I’m going to be trying to keep you up to date with what happens next and I’m happy to answer any questions that you may have to the best of my ability so feel free to ask away.










